The Harvard LAMP Project
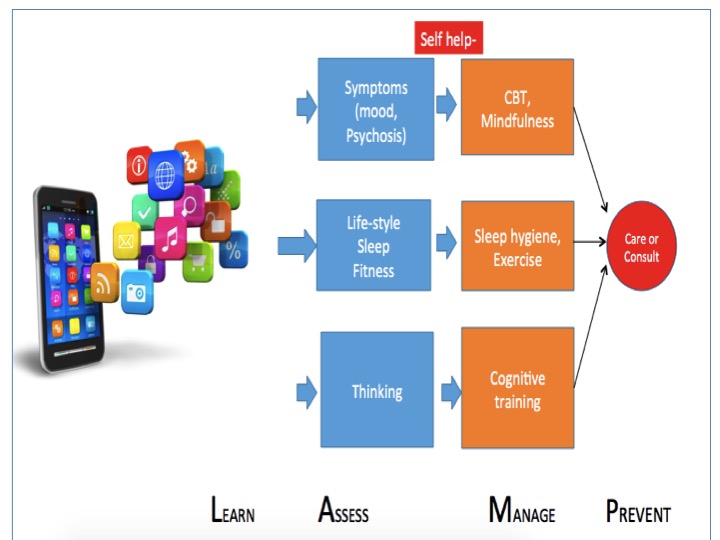
The LAMP (Learn, Assess, Manage, Prevent) project will offer patients, clinicians, and family members new tools and resources to learn about, assess, manage, and help prevent schizophrenia. With the support of the Natalia Mental Health Foundation (formerly the Myrtlewood Foundation) we will create and clinically validate smartphone based care tools built upon scientific and medical evidence. The project will provide patients, clinicians, and family members with access to high quality tools – but with the convenience of a phone based platform.
While there are increasingly more digital and smartphone tools available, LAMP is different. First, few smartphone tools target schizophrenia. Second LAMP is designed solely to help those with schizophrenia and there are no other competing priorities. Thus LAMP is built with data safety in mind and keeps all health information secure. LAMP does not share or sell users health data and let’s user decide if and with whom they want to share data. LAMP is also actionable and does not collect health data for the sake of data alone. Everything that LAMP gathers can be used to guide adjunctive treatments offered on the smartphone or aid in direct clinical care.
Learn: A key first step in effective illness and wellness management is health awareness. LAMP will have built-in an online library of easy to understand education modules that the users have at their fingertips and can interactively navigate and request help resources as needed.
Assess: LAMP will gather several types of clinical data. Through offering surveys on the phone, LAMP will enable real time assessment of mood and thought symptoms. This is important as many mental disorders, including schizophrenia, lead to cognitive and memory deficits so accurately remembering symptoms can be difficult for some. LAMP will also integrate with fitness tracking wrist bands to collect data on sleep duration and quality. Proper sleep is important across all mental health disorders. Heart rate data will also be collected. LAMP will also offer users cognitive tests on the phone via various tap tests and other interactive features. Finally LAMP will also allow users to provide basic information about their current situation such as if they are at home, work, school or alone, with friends, or in a crowd.
Manage: The power of LAMP is, however, not just in data collection that can help better define symptoms but also in its ability to offer a resource and tool in real time and on the go. In response to surveys, LAMP will be able to offer cognitive behavioral therapy exercises from evidence-based treatments for schizophrenia and depression. LAMP will also be able to respond to sleep data and offer real time sleep hygiene coaching to help users achieve better sleep. LAMP will also offer a suite of cognitive remediation therapy tools that will offer a customized set of exercises and tools for each user, based on their unique needs. Cognitive remediation is critical in schizophrenia as it can treat the core domain of cognitive impairment of the illness that our current medications are not as effective in helping with, such as disorganized thoughts.
Prevent: Schizophrenia and other serious mental illness are chronic and recurrent. Relapse prevention is key. LAMP will enable users to record early signs and symptoms so that they can seek help, and so that clinicians can help prevent episodes of illness before they escalate.
We will expand our mobile platform to become a standard research tool for mobile health research and develop broad collaborations with other academic medical centers. We will also add new modules and improve existing ones to ensure our platform remains a trusted, validated, and secure tool for clinical research.
LOCATION
Cambridge MA
Awarded
Fall 2015
The Team
Matcheri Keshavan, MD is Stanley Cobb Professor of Psychiatry at Harvard Medical School, Vice-Chair of Psychiatry at Beth Israel Deaconess Medical Center, and Senior Psychiatric Advisor for Massachusetts Mental Health Center (MMHC) in Boston, MA. Dr Keshavan is closely involved in research in neurobiology (including neuroimaging and sleep studies) of psychosis, especially as it pertains to first episode psychotic disorders, young relatives at risk for psychotic disorders, and in cognitive remediation. He is also pursuing studies of biomarkers in schizophrenia and bipolar disorders. He has published over 600 papers , including four books, and is the chief editor of the Asian Journal of Psychiatry. He has received several awards including the Gaskell Gold Medal of the Royal College of Psychiatrists; Nancy Roschke Certificate for Teaching Excellence of the American Psychiatric Association; teaching awards at the Departments of Psychiatry at Wayne State University and Harvard; the Research Scientist Development Award from the National Institute of Mental Health; the National Alliance for the Mentally Ill of Pennsylvania Psychiatrist of the Year Award; and the Gerard Hogarty Award for Research from the University of Pittsburgh. He is a distinguished Fellow of the American Psychiatric Association; a Fellow of the Royal College of Physicians, Canada; and a Fellow of the Royal College of Psychiatrists, Dr. Keshavan is a board certified psychiatrist, and is the medical director of the PREP-UP clinic providing care for early course psychotic disorder patients at MMHC.
John Torous, MD is a clinical fellow in psychiatry and fourth year psychiatry resident at the Harvard Longwood Psychiatry Residency Training Program. He has a background in electrical engineering and computer sciences and received an undergraduate degree in the field from UC Berkeley before attending medical school at UC San Diego. He has been active in investigating the potential of mobile mental health technologies for psychiatry and helped create his own research apps for the iTunes and Android stores, served a principal investigator on a smartphone depression screening app study, and published numerous papers on the topic. His opinions have been featured in Scientific American, the Boston Globe, and Nature News and he frequently speaks on the topic of technology and mental health at national meetings. He serves as editor-in-chief for the leading academic journal on technology and mental health, JMIR Mental Health (http://mental.jmir.org/), currently leads the American Psychiatric Association’s task force on the evaluation of commercial smartphone apps, co-chairs the Massachusetts Psychiatric Society's Health Information Technology Committee, and in 2014 was awarded an Outstanding Resident Award for research by the National Institute of Mental Health. He is an assistant editor for the Harvard Review of Psychiatry and section editor for the Asian Journal of Psychiatry as well as Psychiatric Times. In 2015 he was selected as one of ten psychiatry residents.
In memoriam: Larry J. Seidman, PhD (d. September 7, 2017) was a clinical psychologist and neuropsychologist, and was Professor of Psychology in the Department of Psychiatry at Harvard Medical School, at the Massachusetts Mental Health Center (MMHC) Public Psychiatry Division of the Beth Israel Deaconess Medical Center (BIDMC) and Massachusetts General Hospital (MGH). He was Vice Chair (Research at MMHC), Public Psychiatry Division of the BIDMC, Director of the Center of Excellence in Clinical Neuroscience and Psychopharmacological Research, and Director of the Neuropsychology Laboratory at MMHC. He was a faculty member of the Clinical and Research Program of the MGH Pediatric Psychopharmacology Unit since 1991. An active researcher, teacher, and clinician, particularly with respect to neurodevelopmental disorders in psychiatry, Dr. Seidman was Principal Investigator at Harvard Medical School on several National Institute of Health grants designed to clarify the etiology and pathophysiology of schizophrenia and is the PI of the Prodrome Treatment and Education grant funded by the Sidney R. Baer, Jr. Foundation, which funds a clinical program oriented to early intervention and prevention of psychotic illnesses. He was also involved in ADHD research over the past two decades. His loss is deeply felt.
Luis R.Sandoval, PhD is Instructor in Psychology, Harvard Medical School, and a at the Public Psychiatry Division at Beth Israel Deaconess Medical Center and at the Commonwealth Research Center. His clinical specialization is in the diagnosis and treatment of adults with severe mental illness, including psychotic and mood disorders. Dr. Sandoval has worked in Mexico, Central America, and in the U.S. and has nearly 14 years of clinical experience. His clinical and research interests include computer-human interaction, cognitive remediation in psychotic disorders, and cross-cultural diagnoses. His current work focuses on the impact that peer social engagement has on cognitive functions in patients with schizophrenia, and how computerized-cognitive interventions could recover cognitive functioning in individuals with psychotic disorders.